The South Carolina Fetal Infant Mortality/Morbidity Review/Human Immunodeficiency Virus (FIMR/HIV) Program aims to improve perinatal HIV prevention systems for women, infants, children, and families. This is achieved through a five-step methodology process:
- Case Identification
- Data Abstraction
- Maternal Interview
- Case Review Team (CRT)
- Community Action Team (CAT)
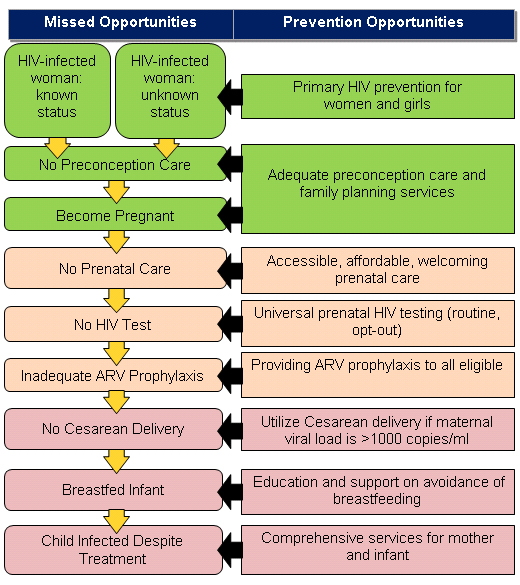
A case is defined as, "HIV-exposed infant/fetus ≥ 24 weeks gestation and < 24 months of age at the time of the review”. Cases for review are prioritized, not randomly selected and are de-identified at the time of review to ensure the confidentiality of mothers and babies. Cases are selected based on key indicators of missed HIV prevention or treatment opportunities, such as:
- HIV-infected infant
- Late maternal HIV diagnosis in the prenatal period
- Lack of, or inadequate, prenatal care
- Lack of maternal HIV treatment or poor viral suppression during pregnancy
- Lack of antiretroviral prophylaxis during labor and delivery
- History of mental health disorders
- History of substance abuse
The SC FIMR/HIV Program reviews up to twelve cases per year to gain the mother’s perspective of her antepartum, intrapartum, and postpartum care. The Case Review Team (CRT) provides recommendations to improve perinatal HIV prevention systems which are then taken to the Community Action Team (CAT). The CAT reviews the recommendations made by the CRT and prioritizes them for action.
For more information and additional resources, please visit the National FIMR/HIV Resource Center at www.fimrhiv.org.
Women and HIV
The Centers for Disease Control and Prevention (2019) estimates that in the United States in 2018, 19% of new HIV diagnoses were among women. Additionally, 1 in 9 women with HIV do not know they have it. In South Carolina, 23% of new HIV diagnoses were among women between 2017-2018. Moreover, Black and African American females are disproportionately affected by HIV than White females. Black and African American women made up 16% of new HIV diagnoses in 2017/2018 compared to 5% among White females and 1% among Hispanic females. In 2018, the perinatal HIV-exposed birth rate for Black and African American women was 10 times higher compared to White women. These disproportionate rates are influenced by several factors, including but not limited to socioeconomic status, poverty, and affordable and accessible quality health care.
About Perinatal HIV
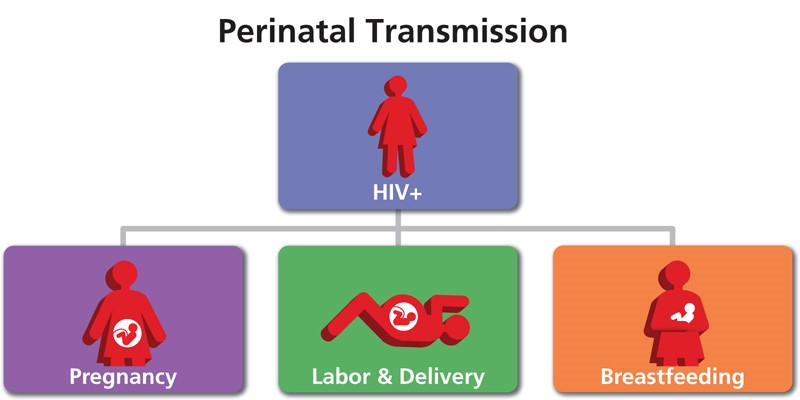
Perinatal HIV transmission can occur during pregnancy, labor/delivery, and breastfeeding. If HIV antibodies are present during the newborn screening test, this means that the mother has HIV/AIDS and that the baby has been exposed to HIV. Not all babies who are exposed to maternal HIV antibodies develop HIV (Baby’s First Test, 2020).
2018 data reported an average of 1 perinatal HIV transmission case and an average of 67 perinatal HIV exposures per year in South Carolina. While progress has been made in significantly reducing these numbers, South Carolina aims to eliminate mother-to-child HIV transmission. The most current data on perinatally acquired and exposed HIV infection can be found in South Carolina's HIV/AIDS Epi Profile.
Contact Us
For more information on the SC FIMR/HIV Program or to join the Case Review Team and/or Community Action Team, email us at fimrhiv@dph.sc.gov
References
- Baby’s First Test. (2020). Human Immunodeficiency Virus. Retrieved from https://www.babysfirsttest.orgnewborn-screening/conditions/human-immunodeficiency-virus
- Centers for Disease Control and Prevention [CDC]. (2019, November 12). HIV and Pregnant Women, Infants, and Children. Retrieved from https://www.cdc.gov/hiv/group/gender/pregnantwomen
- FIMR/HIV Prevention Methodology National Resource Center. (2009). FIMR/HIV Prevention Methodology. Retrieved from http://www.fimrhiv.org
- Figure 1. AIDSinfo. (2020, May 20). Retrieved from https://aidsinfo.nih.gov/understanding-hiv-aids/glossary/810/perinatal-transmission

