Unless you work in the health care field or understand statistics, you may not be familiar with some of the words or labels mentioned in the S.C. Hospital-Acquired Infections Public Reports. On this page, we've tried to explain what some of them mean. Don't worry if it seems like too much to absorb at once. You don't need to know all the terms to understand the reports.
Abbreviations / Acronyms
CDC - Centers for Disease Control and Prevention
CI - Confidence Intervals
CLABSI - Central line-associated bloodstream infection
CMS - Centers for Medicare and Medicaid Services
DHEC - SC Department of Health and Environmental Control
DHHS - Department of Health and Human Services (U.S.)
HAI - Hospital-Acquired Infection
HICPAC - Health Care Infection Control Practices Advisory Committee
HIDA - Hospital Infections Disclosure Act, South Carolina
ICD-9 - International Classification of Diseases, Ninth Revision
MDRO - Multidrug-resistant organism
MRSA - Methicillin-Resistant Staphylococcus aureus
NHSN - National Health Care Safety Network
NQF - National Quality Forum
POA - Present on admission
QIO - Quality Improvement Organization
SCIP - Surgical Care Improvement Project
SHEA - Society for Health Care Epidemiologists of America
SIR - Standardized Infection Ratio
SSI - Surgical site infection
VAP - Ventilator-associated pneumonia
Definition of Terms - HAI Public Reports
Central line: This is a flexible tube that's inserted near a patient's heart or into one of the large blood vessels near the heart. A central line can be used to give fluids, antibiotics, medical treatments such as chemotherapy, and liquid food if a patient is unable to eat or digest food normally. If a central line is inserted incorrectly or not cared for properly, it can cause dangerous bloodstream infections. Central lines are also sometimes called central venous lines, central venous catheters and C-lines.
Central Line-Associated Bloodstream Infection (CLABSI):
When a patient gets a bloodstream infection after having a central line put in (or, in the case of a newborn, an umbilical catheter is also a central line) and the bloodstream infection is not related to an infection in another part of the body it's considered a CLABSI. According to the Centers for Disease Control and Prevention (CDC), an estimated 248,000 CLABSIs occur in U.S. hospitals each year. These bloodstream infections often lead to longer hospital stays, higher costs, and an increased risk of dying. CLABSIs can be prevented through proper insertion and care of the central line. Every time a patient gets an infection that meets the definition of a CLABSI, hospitals must report it to the National Health Care Safety Network (NHSN), defined below.
Central line days: This is the total number of days a central line is in place for patients in surgical, intensive care, and certain other hospital units. The count is performed at the same time each day. Each patient with one or more central lines at the time the count is performed is counted as one central line day.
For example: Five patients on the first day of the month had one or more central lines in place. Similarly, five patients on day 2, two patients on day 3, five patients on day 4, three patients on day 5, four patients on day 6,; and four patients on day 7 had central lines in place. Adding the number of patients with central lines on days 1 - 7 we would have 5 + 5 + 2 + 5 + 3 + 4 + 4 = 28 central line days for the first week. The number of central line days for the month is simply the sum of the daily counts.
CLABSI Infection Rate: To get this rate, we divide the total number of central line-associated bloodstream infections by the number of central line days. That result is then multiplied by 1,000.
The Central Line Utilization Ratio: This ratio comes from dividing the number of central line-days by the number of patient days.
Confidence Intervals (CI) and Standardized Infection Ratios (SIR):
Standardized Infection Ratio
The Standardized Infection Ratio (SIR) is a summary measure used to compare the central line associated bloodstream infection (CLABSI) experience among a group of reported locations or the Surgical Site Infection (SSI) experience among a group of reported procedures to that of a standard population. It is the observed number of infections divided by the expected number of infections.
For HAI reports, the standard population comes from NHSN data reported from all hospitals using the system in the United States. "Expected" is based on historical data for those procedures at the national level.
Understanding the Standardized Infection Ratio (SIR) Statistical Interpretation:
Higher: The facility's SIR was statistically higher than the national SIR.
Lower: The facility's SIR was statistically lower than the national SIR.
Not Different: The facility's SIR was not statistically different from the national SIR.
Confidence Intervals (CIs )
Because we can never obtain a hospital's true "population" data (e.g. all patients for all time), we use statistical procedures to "estimate" various measurements using "sample" data. Since estimates have "variability" we use 95% confidence limits (or intervals) to describe the variability around the estimate. The confidence interval (CI) gives us the range within which the TRUE value will fall 95% of the time, assuming that the sample data are reflective of the true population.
For HIDA reports, the confidence interval is based on the specific number of infections observed in a hospital during the time period in question and on the number of surgeries or patient-days involving a central line that preceded infections.
If two hospitals have different infection rates, but the confidence intervals for the two rates overlap, then it is reasonably possible that the REAL rates are not different from one another. Below is a graphical example of what CIs would look like if they were in graph form. For more information, see the ( Discussion of confidence intervals ) ( pdf )
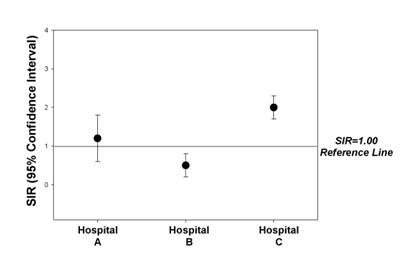
Graph Interpretation:
Hospital A: If the 95% confidence interval crosses over the reference line of 1.0, we conclude that the hospital's infection rate is similar (not significantly different) from "expected" (predicted).
Hospital B: If the 95% confidence interval falls completely below the reference line of 1.0, we conclude that the hospital's infection rate is significantly lower than "expected" (predicted).
Hospital C: If the 95% confidence interval falls completely above the reference line of 1.0, we conclude that the hospital's infection rate is significantly higher than "expected" (predicted).
All conclusions are based on the assumption that the hospital's patient population is similar to the NHSN pooled patient population.
*Please note that the "expected" number of infections does not mean that you expect to get an infection when you go into the hospital for care. The goal is for the hospital is to prevent all HAIs.
Healthcare Associated Infections (HAI):
HIDA reports look at four types of infections that result from common hospital procedures. Other procedures will be phased in over several years. This gradual expansion will give hospitals time to create and refine their own internal data collection processes.
- Surgical Site Infections (SSI): These are infections that result from select surgical procedures. All hospitals where these surgeries are performed must report surgical site infections. The surgeries that must be reported to DHEC are defined by the NHSN and listed in the HAI Public Report.
- Central Line Associated Bloodstream Infections (CLABSI): This includes all central line infections that occur in the hospital units specified by DHEC and defined by the NHSN "locations" listed in the HAI Public Report.
- Ventilator associated pneumonia (VAP): Patients who need mechanical help to breathe have a high risk of developing hospital-acquired pneumonia. Reporting for VAP will be phased in when a standardized definition is developed. A standardized definition will make sure that hospitals are reporting the exact same event and will allow comparison between hospitals.
- Methicillin Resistant Staphylococcus aureus Bloodstream Infections (MRSA BSI): MRSA is a highly contagious germ that does not respond to ordinary antibiotics. Clinical laboratories are already required to report MRSA-positive blood cultures to the "Reportable Conditions" monitoring system operated by DHEC's Bureau of Disease Control. For more information of MRSA, see the "Other" category in the HAI Report.
- Clostridium difficile (C. difficile ) is a type of bacteria that causes severe diarrhea and can be deadly. C. difficile infections usually occur in people who have recently taken antibiotics and have been under medical care. C. difficile is responsible for a spectrum of C. difficile infections (CDI), including uncomplicated diarrhea, pseudomembranous colitis, and toxic megacolon, which can, in some instances, lead to sepsis and even death.
- Ventilator-associated Events (VAE): VAEs are identified by using a combination of objective criteria: deterioration in respiratory status after a period of stability or improvement on the ventilator, evidence of infection or inflammation, and laboratory evidence of respiratory infection.
Hospital Acquired Infection (HAI): For an infection to qualify as an HAI, there must be no evidence that it was present or incubating at the time of hospital admission. A HAI may be confined to one area of the body (localized) or be spread throughout (systemic). It is the body's adverse reaction to the presence of an infectious agent(s) or its toxin(s).
Infection control/prevention processes: These are routine measures to prevent infections that can be used in all health care settings. These steps or principles can be expanded to meet the needs of specialized types of hospitals. Some hospitals make the processes mandatory. Examples include:
- Diligent hand cleaning
- Use of personal protective equipment such as gloves, gowns, and/or masks when caring for patients in selected situations to prevent the spread of infections.
- Use of an infection prevention checklist when putting in central lines. The list reminds health care workers to clean their hands thoroughly; clean the patient's skin before insertion with the right type of soap; wear the recommended sterile gown, gloves and mask; and place sterile barriers around the insertion site, etc.
- Monitoring to ensure that staff are following the proper infection prevention procedures.
Infection Preventionists (IP): These health professionals have special training in infection prevention and monitoring.
Intensive Care Unit (ICU) (also known as Critical Care Unit): ICU's are hospital units that provide intensive observation and treatment for patients either dealing with, or at risk of developing, life threatening problems. Smaller hospitals typically care for both medical and surgical patients in a combined medical/surgical ICU. Larger hospitals typically have separate ICUs for medical patients and surgical patients.
Logistic Regression Model: A logistic regression model is a statistical method used to predict the probability or risk of an occurrence of an event. Logistic regression models make use of several predictor variables that may be either numerical and/or categorical.
National Health Care Safety Network (NHSN): This is the data reporting system that South Carolina hospitals must use to send HAI reports to DHEC twice a year. NHSN is a secure, internet-based surveillance (monitoring and reporting) system. Among other features, the network offers integrated patient and health care worker safety surveillance systems. The NHSN is managed by the CDC's Division of Health Care Quality Promotion.
Hospitals submit specific infection and procedural information to NHSN that is needed to calculate infection rates for each procedure. Hospitals must assign rights to DHEC to collect the data from NHSN so that the information can be reported to the public. DHEC selected this reporting system with the advice of the HIDA Advisory Committee.
NHSN Patient Safety Protocol Manual: This contains standardized surveillance definitions and data collection methods that are essential for fairly reporting hospital infection rates.
Standardized Infection Ratio: (See Confidence Interval for combined description of both definitions.)
Standardized Infection Ratio (SIR) Statistical Method: This indirect standardization method accounts for differences in the risk of surgical site infections among a group of procedures.
A SIR is the number of observed infections divided by the number of expected infections. The expected number is based on the national average, the number of procedures performed by a hospital, and historical data for those procedures.
- A SIR of 1.0 means the observed number of infections is equal to the number of expected infections.
- A SIR above 1.0 means that the infection rate is higher than that found in the "standard population." For HAI reports, the standard population comes from data reported by the hundreds of U.S. hospitals that use the NHSN system. The difference above 1.0 is the percentage by which the infection rate exceeds that of the standard population.
- A SIR below 1.0 means the infection rate is lower than that of the standard population. The difference below 1.0 is the percentage by which the infection rate is lower than that experienced by the standard population.
The number of expected infections is calculated by multiplying the number of procedures (at each hospital) by the NHSN Pooled Mean Rate. The result is divided by 100 (to remove the percent).
The SIR is found by dividing the sum of the observed number of SSIs by the sum of the expected number of SSIs across the different procedures.
*Please note that the "expected" number of infections does not mean that you expect to get an infection when you go into the hospital for surgery. The goal is for the hospital is to prevent all HAIs.
Surveillance: The process of finding and documenting infections.
- Active Surveillance: This includes, but is not limited to, active, patient-based, prospective surveillance by a trained infection control professional (IP). The IP seeks out infections during a patient's stay by screening a variety of data sources. The sources may include laboratory, pharmacy, admission/discharge/transfer, radiology/imaging, and pathology databases; and patient charts, including history and physical exams notes, nurses/physician notes, and temperature charts. The complete definition for surveillance, including how to capture denominator data to calculate infection rates, is found in each module of the NHSN Manual: Patient Safety Protocols.
- Post discharge surveillance: This is the process IPs use to seek out infections after patients have been discharged from the hospital. It includes screening a variety of data sources, including re-admissions and emergency department visits.
Surgical Site Infection (SSIs):
SSIs are infections that occur as the result of surgeries defined in the NHSN Patient Safety Protocols. The definition addresses inpatient/outpatient status, type of incision, type of operating room, and other situations. For example, under the "other" category, burn wounds are excluded from the definition of a reportable SSI.
All patients undergoing surgical procedures that are included in the definition are counted and monitored for infection.
HIDA also requires hospitals to report "risk adjusted" infection rates. The following definitions explain how the rates are calculated and which patient risk factors are considered in risk adjustments.
- SSI Rate: Surgical site infection rates per 100 operative procedures are found by dividing the number of SSIs by the number of total number of specific operative procedures within a given reporting period. The results are then multiplied by 100. These calculations are performed separately for each type of surgical procedure. They are listed by risk index (see definition, below). (Standardized infection ratios can also be calculated using indirect standardization or multivariate models.)
- SSI Basic Risk Index: This is a score used to predict a surgery patient's risk of acquiring a surgical site infection. The risk index score, ranging from 0 to 3, reveals how many of these risk factors are present:
- The anesthesiologist has given the patient an American Society of Anesthesiologists' (ASA) physical status classification score of 3, 4, or 5.
- The operation is classified as contaminated or dirty/infected.
- The operation lasts longer than the duration cut point hours. (See below for definition.)
- ASA Score: This is an assessment by the anesthesiologist of the patient's physical condition prior to surgery. It uses the American Society of Anesthesiologist' (ASA) Classification of Physical Status. It's one of the factors that helps determine a patient's risk of acquiring a surgical site infection (a patient's SSI Basic Risk index). Here is the ASA scale:
- Normally healthy patient
- Patient with mild systemic disease
- Patient with severe systemic disease that is not incapacitating
- Patient with an incapacitating systemic disease that is a constant threat to life
- Moribund patient who is not expected to survive with or without the operation.
- Wound Class: This is an assessment of the degree of contamination of a surgical wound at the time of the operation. The wound class system used in the NHSN is an adaptation of the American College of Surgeons wound classification system. Wounds are divided into four classes:
- Clean: An uninfected operative wound in which no inflammation is encountered and the respiratory, digestive, genital, or uninfected urinary tracts are not entered. In addition, clean wounds are primarily closed and, if necessary, drained with closed drainage. Operative incisional wounds that follow blunt trauma should be included in this category if they meet the criteria.
- Clean-Contaminated: Operative wounds in which the respiratory, digestive, genital, or urinary tracts are entered under controlled conditions and without unusual contamination. Specifically, operations involving the biliary tract, appendix, vagina, and oropharynx are included in this category, provided no evidence of infection or major break in technique is encountered.
- Contaminated: Open, fresh, accidental wounds. In addition, operations with major breaks in sterile technique (e.g., open cardiac massage) or gross spillage from the gastrointestinal tract, and incisions in which acute, nonpurulent inflammation is encountered are included in this category.
- Dirty or Infected: Includes old traumatic wounds with retained devitalized tissue and those that involve existing clinical infection or perforated viscera. This definition suggests that the organisms causing postoperative infection were present (in the operative field) before the operation.
Duration Cut Point: Different procedures have different duration cut points. When a surgery lasts longer than the duration cut point time assigned to that type of operation, infection risks may increase. Cut points are assigned based upon the time that the majority (75%) of those procedures take to perform. The duration cut point is measured in minutes and is the time between the skin incision and skin closure.
For example: The duration cut point for a coronary bypass graft (chest and donor incision) is five hours and one minute(301 minutes). For an abdominal hysterectomy, the duration cut point is two hours and twenty three minutes(143 minutes).
Validation:
For HIDA, validation is the process of making sure the HAI data reported to NHSN are complete and accurate. That includes SSIs, the total numbers of surgical procedures performed, central line days, and patient information to assign risk scores.
The purpose of the validation visits are to:
- Assess the accuracy and quality of the data submitted to the NHSN
- Provide hospitals with information to help them use the data system.
- Provide education to the IPs and other hospital staff (or Anesthesia and IT) if necessary to improve data accuracy and quality
- Teach the IPs how to validate the written or electronic data they receive from other departments such as the Operating Room.
- Look for unreported HAIs
- Assess selected infection control processes
- Make recommendations for improvements if data accuracy and/or quality issues are discovered.